
This really happened: A woman had her appendix removed and was billed $17,995 by the surgeon1.
Yes, the situation was an emergency and yes, the surgeon was out-of-network. But the woman was charged 20 times more than the average cost for an in-network surgeon performing the same procedure2.
The same woman was also billed $8,500 by the surgeon’s out-of-network assistant. That’s 60 times the average payment for an in-network provider1,2.
Since the payment rates for in-network providers – including doctors, hospitals, labs, tests, and procedures — are established and agreed upon in advance, this kind of serious balance billing occurs only when people go out-of-network. In simple terms, a balance bill is the difference between the out-of-network provider’s full charge for a service and the amount that’s allowed by your plan.
Perception vs. reality
Members should expect out-of-network health care costs to be higher. But the question is: How much higher? Sometimes what’s being billed seems like an arbitrary amount and it’s difficult for members to know what they should expect to pay.
Unfortunately, balance billing happens. While most providers bill reasonable amounts, some providers have learned they’ll sometimes get paid what they’re asking.
The perception most people have is that health care providers almost always charge rates that are reasonable and consistent with the marketplace. Sorry to burst any bubbles, but that’s a myth. Although balance billing is the exception and not the rule, it’s not uncommon.
Balance medical billing is not always an accident
Sometimes balance billing happens by accident. And no wonder, since there are nearly 70,000 diagnosis codes and over 71,000 procedure codes to sift through3. But there are times when balance billing may be intentional.
Some providers deliberately remain out of health insurer networks because they often make more money by doing so. When a provider is in-network, they’ve signed a pricing contract with the insurance company and agree to a set payment for their services. Out-of-network providers might try to bill and collect whatever rate they want.”
What can you do if you suspect you’re being balance billed for out-of-network health care? One step Naviguard suggests is to carefully review your Explanation of Benefits. You can learn a lot about this useful document in this article.
If you’re a UnitedHealthcare member and your employer has arranged for your plan to include Naviguard, you have a service you can turn to if you get an out-of-network balance medical bill. Naviguard experts will review the bill and work with the health care professional to reduce or eliminate the balance medical bill — at no additional cost to you.
Learning the lingo of health insurance
The better you understand your medical bills, the less likely you’ll overpay if you’re charged too much. The Explanation of Benefits (EOB) you’re sent after receiving a health care service provides much useful information – including the full price you provider is charging your insurance company and how much you may be responsible for paying.
Not surprisingly, most people don’t know what a balance medical bill is. Or how a deductible works. Or the difference between a copayment and coinsurance.
There are many steps you can take to become a savvy health care consumer. One is to learn some of the lingo of health Insurance. This glossary can help. It does a wonderful job of defining the terms you need to know in plain, clear language to help you make informed decisions and make sense of your medical bills. Knowledge is power. With Naviguard, you’ll get the support you need to understand out-of-network balance medical bills and resolve them.
RESOURCES
- Learn how Naviguard can help members negotiate of out-of-network balance medical bills
- Learn how Naviguard can help employers manage out-of-network health care costs
- Discover the experiences of others who have benefited from Naviguard's expertise in balance medical bill negotiation
REFERENCES
- Naviguard case data
- Compared to the Fair Health Benchmark allowed
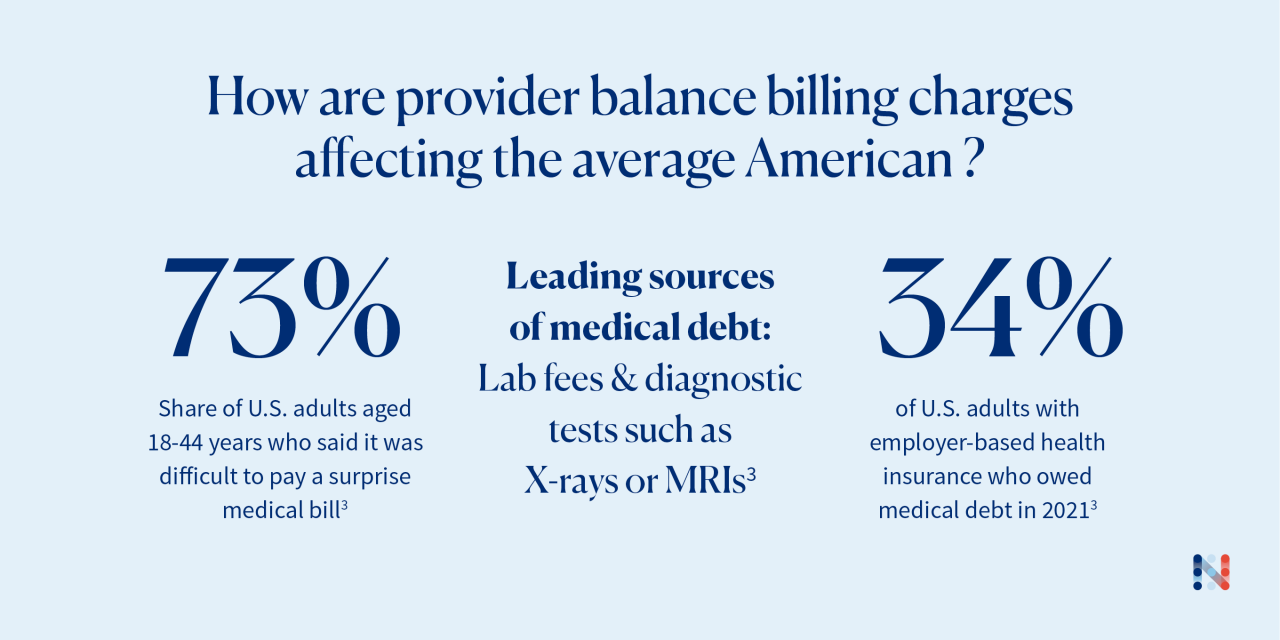
- Vankar, Preeti. “Medical Debt in the U.S. - Statistics & Facts | Statista.” Statista, 9 Jan. 2023

